- Researchers from the University of Sheffield and the University of Eastern Finland confirm being overweight is an additional burden on brain health and it may exacerbate the disease
- Maintaining a healthy weight could help preserve brain structure in people who are already experiencing mild Alzheimer’s disease
New research from the University of Sheffield has found being overweight is an additional burden on brain health and it may exacerbate Alzheimer’s disease.
The pioneering multimodal neuroimaging study revealed obesity may contribute toward neural tissue vulnerability, whilst maintaining a healthy weight in mild Alzheimer’s disease dementia could help to preserve brain structure.
The findings, published in The Journal of Alzheimer’s Disease Reports, also highlight the impact being overweight in mid-life could have on brain health in older age.
The diseases that cause dementia such as Alzheimer’s and vascular dementia lurk in the background for many years, so waiting until your 60s to lose weight is too late. We need to start thinking about brain health and preventing these diseases much earlier.
Professor Annalena Venneri
Professor of Clinical Neuropathy at the University of Sheffield
Lead author of the study, Professor Annalena Venneri from the University of Sheffield’s Neuroscience Institute and NIHR Sheffield Biomedical Research Centre, said: “More than 50 million people are thought to be living with Alzheimer’s disease and despite decades of ground breaking studies and a huge global research effort we still don’t have a cure for this cruel disease.
“Prevention plays such an important role in the fight against the disease. It is important to stress this study does not show that obesity causes Alzheimer’s, but what it does show is that being overweight is an additional burden on brain health and it may exacerbate the disease.”
She added: “The diseases that cause dementia such as Alzheimer’s and vascular dementia lurk in the background for many years, so waiting until your 60s to lose weight is too late. We need to start thinking about brain health and preventing these diseases much earlier. Educating children and adolescents about the burden being overweight has on multimorbidities including neurodegenerative diseases is vital.”
Researchers from the University of Sheffield and the University of Eastern Finland examined MRI brain scans from 47 patients clinically diagnosed with mild Alzheimer’s disease dementia, 68 patients with mild cognitive impairment, and 57 cognitively healthy individuals.
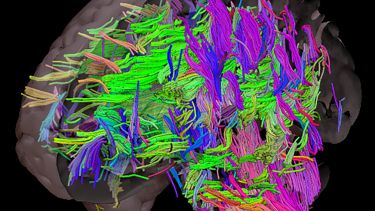
The novel study used three complementary, computational techniques to look at the anatomy of the brain, blood flow and also the fibres of the brain.
The international team compared multiple brain images and measured differences in local concentrations of brain tissues to assess grey matter volume - which degenerates during the onset of Alzheimers - white matter integrity, cerebral blood flow and obesity.
In mild dementia patients, a positive association was found between obesity and grey matter volume around the right temporoparietal junction. This suggests obesity might contribute toward neural vulnerability in cognitively healthy individuals and those with mild cognitive impairment.
The study also found that maintaining a healthy weight in mild Alzheimer’s disease dementia could help preserve brain structure in the presence of age and disease-related weight loss.
Joint author of the study, Dr Matteo De Marco from the University of Sheffield’s Neuroscience Institute, said: “Weight-loss is commonly one of the first symptoms in the early stages of Alzheimer’s disease as people forget to eat or begin to snack on easy-to-grab foods like biscuits or crisps, in place of more nutritional meals.
“We found that maintaining a healthy weight could help preserve brain structure in people who are already experiencing mild Alzheimer’s disease dementia. Unlike other diseases such as cardiovascular disease or diabetes, people don’t often think about the importance of nutrition in relation to neurological conditions, but these findings show it can help to preserve brain structure.”
The study was conducted in collaboration with the University of Eastern Finland. Professor Hilkka Soininen, joint author of the paper, said: “The results emphasise different perspectives on lifestyle and nutrition in the prevention and treatment of Alzheimer’s disease. It’s important to avoid obesity for brain health, but for patients with Alzheimer's disease, it is essential to take care of proper nutrition and maintain a healthy weight.”
The Neuroscience Institute at the University of Sheffield brings together leading experts in medicine, science and engineering to better understand the nervous system and tackle the biggest challenges in neuroscience.
Notes to editors
NIHR Sheffield Biomedical Research Centre
The National Institute for Health Research (NIHR) is the nation’s largest funder of health and care research. The NIHR:
● Funds, supports and delivers high quality research that benefits the NHS, public health and social care
● Engages and involves patients, carers and the public in order to improve the reach, quality and impact of research
● Attracts, trains and supports the best researchers to tackle the complex health and care challenges of the future
● Invests in world-class infrastructure and a skilled delivery workforce to translate discoveries into improved treatments and services
● Partners with other public funders, charities and industry to maximise the value of research to patients and the economy
The NIHR was established in 2006 to improve the health and wealth of the nation through research, and is funded by the Department of Health and Social Care. In addition to its national role, the NIHR commissions applied health research to benefit the poorest people in low- and middle-income countries, using Official Development Assistance funding.
This work uses data provided by patients and collected by the NHS as part of their care and support and would not have been possible without access to this data. The NIHR recognises and values the role of patient data, securely accessed and stored, both in underpinning and leading to improvements in research and care.
Contact
For more information, please contact: