The deceptive hormone essential for health, but helping pancreatic cancer
Pancreatic cancer is one of the world’s most aggressive cancers. But what if the hormone that allows it to grow is the key to stopping it in its tracks?
Our bodies are loaded with an array of molecules and compounds whose functions are to keep us alive. It’s not often that one of those substances is not just a friend, but a foe. But the hormone adrenomedullin — which regulates blood pressure and supports the growth of pancreatic cancer — is both. Recent research from the University of Sheffield has discovered that the dual nature of this hormone could be what we need to defeat the fifth most deadly cancer, with further applicability in other ‘hard to treat’ cancer types.
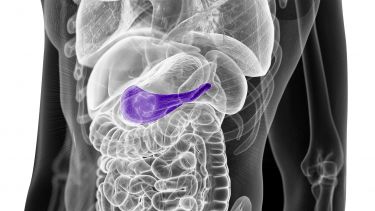
Pancreatic cancer rarely has symptoms in its early stages and those that do occur - like non-specific pain, indigestion and weight loss - are often mistaken for other illnesses. The location of the pancreas also makes it challenging to detect. It’s position at the back of the abdomen behind other organs makes it hard for doctors to feel during routine examinations. Even patients diagnosed early have very poor outlook.
Coupled with its aggressive nature, by the time the cancer is detected it’s often spread into surrounding tissue and other parts of the body. This makes it incredibly difficult to remove surgically; leaving unpleasant chemotherapy as the remaining treatment method. But pancreatic cancer tumours are prepared for this. They’re surrounded by a network of non-cancerous cells which can form a fibrous protective barrier. The result is that over the last few decades pancreatic cancer treatment has progressed very little. So how do you treat the seemingly untreatable?
Professor Tim Skerry from the University of Sheffield’s new biotech spin-out company, Modulus Oncology, is dedicated to developing a treatment. “More than 20 years ago I read a research paper about the unusual receptors for the hormone adrenomedullin. This hormone acts on two distinct receptors rather than one,” explains Tim. The Sheffield team’s discovery of ways to block the receptor involved in cancer progression set in motion the work that has led to a potential new treatment for pancreatic cancer.
Adrenomedullin’s two receptors play dramatically different roles. One lowers our blood pressure to keep it at a safe level, stimulates the growth of new blood vessels and increases the tolerance of cells to stress. But this deceptive hormone has another function. It stimulates cancer cells to multiply much quicker and to live longer so tumours grow faster overall. Adrenomedullin also helps to create a supportive environment for the tumour to grow and spread by reducing the body’s defence mechanisms. So how is one hormone capable of doing so much good for the body, and so much bad?
Through their research Tim and the team have been able to show that there are two distinct protein receptors on the adrenomedullin hormone. Receptors act like a key-operated switch on the outside of a cell — a process comparable to a piece of a jigsaw filling an identically shaped space in a puzzle. When the receptor binds to a hormone (the key in this analogy), it activates biological functions inside the cell. The two separate receptors for adrenomedullin allow the hormone to activate different processes in cells. In adrenomedullin’s case, one receptor is responsible for physiological functions like controlling blood pressure, while the other receptor is responsible for many of the hormone’s functions in cancer.
Our research has been successful in designing a piece to fit into nature’s jigsaw that blocks the adrenomedullin receptor related to cancerous functions without affecting blood pressure regulation.
Professor Tim Skerry
Co-Founder and Chief Scientific Officer (CSO), Modulus Oncology
Current pancreatic cancer treatment methods like chemotherapy are only suitable for a very small number of patients due to the significant side effects, and they can’t be given to frail patients at all. Radiotherapy is also only of limited use, targeting a small number of cancerous cells and not those that have spread to other parts of the body. However, the Sheffield team’s research has now led to a potential new pancreatic cancer drug which has benefits over these more traditional treatment methods that appears to have potent effects but a very low likelihood of side effects.
Until now, the treatment has been tested in mice. However, with the help of Cumulus Oncology, an oncology drug accelerator company - Tim and the team’s treatment is well on the way to becoming a reality. Cumulus has provided support in the first stages of commercialising their drug discovery by co-creating Modulus Oncology. The aim of Cumulus is to develop new treatments that target the unmet needs of specific cancer patient populations. And Tim’s research is a perfect fit for this due to the pressing need for a life-extending treatment for pancreatic cancer. With applicability in other ‘hard-to-treat’ cancers, the scope for further patient benefit also exists.
“When the Sheffield team’s research was presented to us as a potential commercialisation opportunity we realised it had to be done. We were really impressed with the scientific rationale behind the project. The fact that the team had collaborated with medicinal and organic chemists and engaged with industry experts from so early on really added to the potential of the research,” explains Clare Wareing, founder of Cumulus and Modulus Oncology’s Chief Business Officer.
For Tim the motivation to make this research a commercial success falls a little closer to home. “As a researcher it’s normal to make small advances that contribute to society and benefit patients. For me, the last five years and spinning out a company has catapulted our work towards the possibility of generating real improvements in treatment for patients.”
The next stage for Modulus Oncology and the team is to test the molecules as drugs in humans to demonstrate they’re safe and that the treatment is effective. Alongside this, Tim and the team are also studying other rare types of cancer where treatment options are limited. Here, their new treatment could provide a potential benefit to those other tumour types and extend more patients’ lives.
The outlook for pancreatic cancer patients has hardly changed over the last 30 years. But the asset we have at Modulus Oncology is giving us the opportunity to do something about this huge unmet medical need and improve patient outcomes in a range of cancer types.
Clare Wareing
Chief Business Officer, Modulus Oncology
As cases of pancreatic cancer continue to increase worldwide there has never been a more appropriate time for a new treatment. The invention of a new drug molecule is just the first step in a long process, from bench to bedside. However, this new development could lead the way for a treatment for pancreatic cancer patients worldwide.
Written by Alicia Shephard, Research Marketing and Content Coordinator
Graphics by Ella Marke, Visual Designer
Meet the team
Tim Skerry, Co-Founder and Chief Scientific Officer (CSO)
Gareth Richards, Co-Founder and VP of Preclinical Sciences
Alan Wise, Chief Executive Officer
Clare Wareing, Chief Business Officer
Keith Murdoch, Chief Financial Officer
Glen Clack, Chief Medical Officer
Manuelle Debunne, Director of Preclinical programmes
Further information
Key research
Discovery of a First-in-Class Potent Small Molecule Antagonist against the Adrenomedullin-2 Receptor
Funders
For further information contact:
Amy Pullan
Media Relations Officer
University of Sheffield
+44 114 222 9859
a.l.huxtable@sheffield.ac.uk